Discover how managing sleep apnea can positively impact your life expectancy and overall wellness. Sleep Apnea Life Expectancy: Explore effective treatments, lifestyle changes, and the latest research advancements to conquer sleep apnea and thrive.
Table of Contents

Introduction
Sleep apnea is a prevalent sleep disorder characterized by repeated interruptions in breathing during sleep. These interruptions, known as apneas, significantly affect the quality of sleep and overall health, posing serious health risks if left untreated. Understanding sleep apnea is crucial as it impacts millions worldwide, influencing their health, lifestyle, and even life expectancy.
This disorder is typically underdiagnosed, which means many people may be unaware they suffer from it. It manifests in several ways, including obstructive sleep apnea (OSA), the most common form, where the airway becomes physically blocked during sleep, and central sleep apnea, where the brain fails to properly control breathing during sleep.
The implications of untreated sleep apnea extend beyond mere sleep disruption. Individuals with untreated sleep apnea are at increased risk for various complications, including cardiovascular diseases, stroke, and diabetes. Moreover, it significantly impacts mental health, leading to impaired cognitive functions and emotional disturbances.
The following sections will explore the epidemiology of sleep apnea, its impacts on life expectancy, associated medical complications, and the available treatment options. By the end of this post, you should have a comprehensive understanding of sleep apnea and its profound effect on life expectancy, emphasizing the importance of early diagnosis and management. Whether for yourself or someone you care about, recognizing the signs of sleep apnea can be a critical step towards improving health outcomes and quality of life.
What is Sleep Apnea?
Sleep apnea is a serious sleep disorder where a person’s breathing repeatedly stops and starts during sleep. This condition can lead to significant health issues and affects daily life due to fatigue and other symptoms. The primary types of sleep apnea are:
- Obstructive Sleep Apnea (OSA): The most common form, OSA occurs when the throat muscles intermittently relax and block the airway during sleep. It is most often seen in people who are overweight, though it can affect anyone.
- Central Sleep Apnea (CSA): Unlike OSA, CSA occurs when the brain doesn’t send proper signals to the muscles that control breathing. This type of sleep apnea can be associated with certain medical conditions, including conditions that affect the brainstem, heart failure, and stroke.
- Mixed Sleep Apnea: This is a combination of both obstructive and central sleep apnea.
Symptoms
The symptoms of sleep apnea can vary depending on the type but commonly include:
- Loud snoring
- Episodes of breathing cessation during sleep
- Abrupt awakenings accompanied by gasping or choking
- Morning headache
- Daytime sleepiness and fatigue
- Difficulty concentrating during the day
- Mood changes, such as depression or irritability
- High blood pressure
- Nighttime sweating
Diagnosis
Diagnosing sleep apnea usually involves an overnight sleep study called a polysomnography, which records brain waves, blood oxygen levels, heart rate, breathing patterns, and eye and leg movements. A simpler test, known as a home sleep apnea test, measures airflow, breathing patterns, and blood oxygen levels and can be conducted in the comfort of one’s home.
Understanding sleep apnea and getting an appropriate diagnosis are crucial for effective management. With the right treatment, individuals can significantly reduce the risk of health complications and improve their quality of life. The following sections will delve deeper into how sleep apnea affects life expectancy and what can be done to manage this condition effectively.
Suggested Devices 1

【Open Mouth Snoring Solution】: The chin strap for snoring are made of upgraded high-quality soft, elastic, durable, breathable material without odor. Easy to put on and very comfortable to sleep in. (NOTE:This chin strap is only suitable for snoring caused by open mouth exhalation.)
【Adjustable Chin Strap For Snoring】: The chin strap for snorers has a Velcro length of 6.2 inches. The size can be adjusted to a greater extent according to the size of your face. Thickened design is more durable.
【Breathable and Washable】: The snore headband chin strap is perfect breathability. Quickly dissipate heat, there will be no hot feeling during sleep. Do not dry your mouth and throat. Support repeated use, you can clean it regularly to refresh it. You can sleep comfortably without snoring all night.
Epidemiology of Sleep Apnea
Sleep apnea is a widespread condition affecting millions of people worldwide, with its prevalence increasing significantly over the past few decades. This increase is largely attributed to the rising rates of obesity, a key risk factor for obstructive sleep apnea (OSA), the most common form of the disorder. Here are some key aspects of the epidemiology of sleep apnea:
Prevalence
- Global Reach: An estimated 936 million adults aged 30-69 years are affected by mild to severe obstructive sleep apnea globally. The prevalence is higher in men than in women, although the gap narrows after women reach menopause.
- United States: In the U.S., it is estimated that 22 million Americans suffer from sleep apnea, with 80 percent of moderate to severe OSA cases going undiagnosed.
Risk Factors
Several factors increase the likelihood of developing sleep apnea:
- Obesity: Excess body weight significantly increases the risk of OSA, as fat deposits around the upper airway can obstruct breathing.
- Age: The risk of sleep apnea increases with age, peaking in individuals aged 50-60 years.
- Gender: Men are two to three times more likely to have sleep apnea than women. However, the risk for women increases and may surpass that of men in postmenopausal stages.
- Ethnicity: Certain ethnic groups, including Hispanics and African-Americans, are at higher risk compared to others.
- Family History and Genetics: Having family members with sleep apnea can increase one’s risk, suggesting a genetic basis.
Impact of Undiagnosed Sleep Apnea
The large number of undiagnosed sleep apnea cases is a major public health concern. People with untreated sleep apnea face higher risks of several serious health issues, including hypertension, cardiovascular disease, diabetes, and accidents caused by daytime sleepiness. Moreover, sleep apnea significantly impacts life expectancy when left untreated, which underscores the importance of awareness and diagnosis.
The epidemiological data clearly indicate that sleep apnea is not only a common health issue but also a severe one that can have significant impacts on public health and individual well-being. Addressing this condition with appropriate therapeutic interventions is crucial for reducing its widespread public health ramifications. The subsequent sections will explore the medical complications associated with sleep apnea and the available treatment options that can help mitigate these effects.

Sleep Apnea Life Expectancy: Link to Life
Sleep apnea is more than just a nuisance that disrupts sleep; it has serious implications for life expectancy and overall health. Research has shown that untreated sleep apnea can lead to a range of life-threatening conditions, ultimately shortening life span if not properly managed.
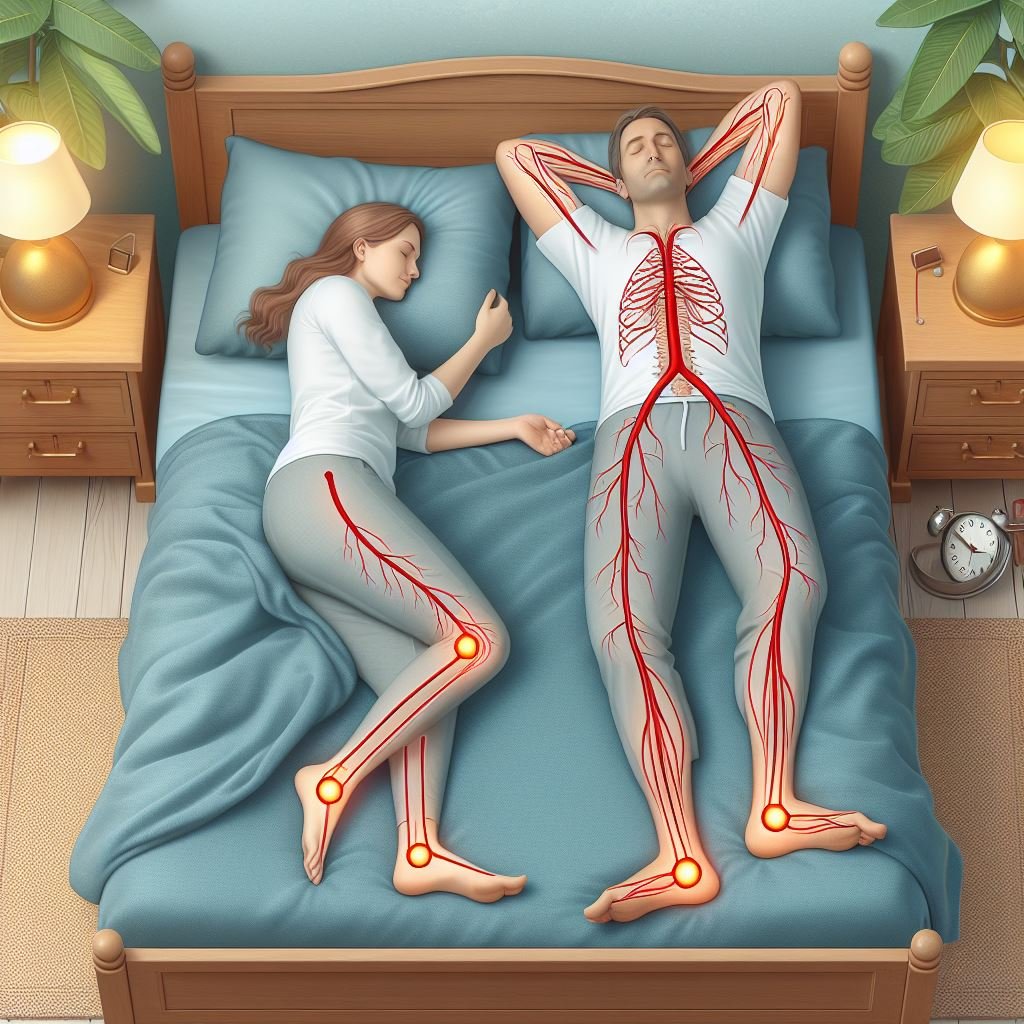
Impact on Health
Obstructive Sleep Apnea (OSA) is particularly detrimental due to its ability to induce intermittent hypoxia (repeated episodes of low oxygen levels in the blood) and sleep fragmentation. Both of these conditions trigger a cascade of physiological disturbances that have profound health impacts:
- Cardiovascular Disease: Sleep apnea is strongly linked with an increased risk of high blood pressure, coronary artery disease, heart attack, and stroke. The strain of repeatedly waking up during the night, along with low oxygen levels, stresses the heart and vascular system.
- Heart Rhythm Irregularities: People with sleep apnea are more likely to experience arrhythmias (irregular heartbeats), which can be severe and are sometimes linked to sudden death.
- Diabetes: The disrupted oxygen flow can also lead to type 2 diabetes by influencing insulin resistance caused by chronic sleep disruption and intermittent hypoxia.
Quantifying the Impact on Life Expectancy
Several studies have attempted to quantify the impact of sleep apnea on mortality:
- General Mortality Risk: Research indicates that severe sleep apnea increases the overall mortality risk by up to three times, particularly from cardiovascular problems.
- Heart-Related Deaths: Patients with untreated sleep apnea have a higher rate of death from heart-related issues compared to those without sleep apnea.
- Life Expectancy Reduction: On average, severe untreated sleep apnea can reduce life expectancy by up to 12 years, depending on the presence of other conditions such as obesity, diabetes, and cardiovascular disease.
Read More: Understanding Deviated Septum Sleep Apnea: Breathe Easy, Sleep Sound
Benefits of Treatment
Treating sleep apnea can mitigate these risks significantly:
- CPAP Therapy: Continuous Positive Airway Pressure (CPAP) therapy, the most common treatment for moderate to severe sleep apnea, helps keep the airways open and can significantly reduce the risk of heart problems and improve mortality rates.
- Lifestyle Changes: In addition to medical treatments, lifestyle changes such as weight loss, exercise, and alcohol/tobacco cessation are crucial. They not only help manage sleep apnea but also improve overall cardiovascular health and life expectancy.
Understanding the link between sleep apnea and life expectancy underscores the importance of early diagnosis and proactive management of this common but dangerous disorder. Ignoring sleep apnea can lead to a significantly diminished quality of life and premature death, while addressing it can restore health and vitality. The following sections will delve into the specific medical complications associated with sleep apnea and explore effective treatment options in more detail.

Medical Complications Associated with Sleep Apnea
Sleep apnea does not just disrupt sleep; it can lead to severe health issues if left untreated. The intermittent hypoxia (low blood oxygen levels) and sleep fragmentation characteristic of sleep apnea trigger various systemic complications:
Cardiovascular Issues
Hypertension: Frequent night-time awakenings and oxygen deprivation can cause hormonal changes that increase blood pressure. Consistently high blood pressure, or hypertension, is common in people with untreated sleep apnea.
Heart Disease: The stress on the cardiovascular system from fluctuating oxygen levels increases the risk of heart disease. This includes coronary artery disease and an increased risk of heart attack.
Heart Failure and Arrhythmias: Sleep apnea disrupts the balance of the cardiovascular system, which can lead to heart failure. It is also linked with irregular heart rhythms, such as atrial fibrillation, which can be dangerous and are associated with stroke.
Respiratory Complications
While obstructive sleep apnea directly affects breathing, it can also exacerbate other respiratory conditions, including chronic obstructive pulmonary disease (COPD) and asthma, leading to more frequent and severe attacks.
Metabolic Disorders
Type 2 Diabetes: The stress and variability in glucose metabolism associated with sleep apnea can lead to insulin resistance, which is a precursor to type 2 diabetes. Studies show that treating sleep apnea can help improve blood sugar levels and insulin sensitivity.
Neurological Effects
Sleep apnea can impact brain structure and function, leading to cognitive decline, memory loss, and decreased concentration. Patients often experience mood swings, anxiety, and depression, significantly affecting their mental health and quality of life.
Other Complications
Complications with Medications and Surgery: People with sleep apnea may be more likely to experience complications following surgery, particularly because sedatives and anesthesia can worsen apnea episodes.
Liver Problems: Nonalcoholic fatty liver disease (NAFLD), which involves high liver enzyme levels and liver scarring, appears to be more common in people with sleep apnea. The severity of NAFLD correlates closely with the severity of apnea.
Sleep-Deprived Partners: The loud snoring that often accompanies sleep apnea can also significantly affect a partner’s sleep quality, leading to a strain in relationships and individual health problems for the partner.
The wide array of health risks associated with sleep apnea highlights the critical need for diagnosis and treatment. Addressing the disorder can help alleviate or even reverse some of these complications, improving overall health and longevity. The next sections will explore treatment options that are effective in managing sleep apnea and reducing the risk of these serious complications.
Read More: Sleep Apnea Without Snoring? Don’t Suffer in Silence
Psychological and Neurological Impacts
Sleep apnea affects not only physical health but also mental and neurological functions. The repeated interruptions in sleep and chronic oxygen deprivation can have profound effects on brain health and psychological well-being.
Cognitive Impairment
Memory Loss: Sleep is critical for memory consolidation; the fragmented sleep experienced by those with sleep apnea can lead to significant deficits in both short-term and long-term memory.
Impaired Cognitive Function: Chronic sleep deprivation impacts cognitive flexibility, decision-making, and problem-solving skills. This cognitive decline can affect job performance and daily activities, leading to decreased quality of life.
Decreased Alertness: Interruptions in sleep impair the brain’s ability to sustain attention. Individuals with sleep apnea often experience severe daytime drowsiness, which increases the risk of accidents while driving or operating machinery.
Suggested Devices 2

【 Advanced Anti-Snoring Technology】Nasal Dilators for Breathing specially designed for those suffering from shortness of breath and nasal congestion. Designed to maximize the airflow to improve breathing and eliminate snoring by dilating nostrils,stimulating acupuncture points, and dredging the airway.
【4 Sizes】 Four different sizes of nasal dilator to fit anyone.The matching box provides excellent protection against dust and dirt and makes the product more durable. Perfect for taking with you so you can use it whenever you want.
【Easy to Clean and Reusable】Maintain your snore-free nights effortlessly with Nasal dilator. These high-quality nasal plugs are easy to clean and can be used again and again, providing long-lasting relief without the need for frequent replacements.
Mental Health Issues
Depression and Anxiety: The chronic tiredness associated with sleep apnea can lead to mood disorders such as depression and anxiety. The stress of constant fatigue and other health complications can exacerbate these conditions.
Irritability and Mood Swings: Sleep apnea can cause significant mood instability. Sufferers often report increased irritability and emotional reactivity, complicating personal and professional relationships.
Neurological Consequences
Brain Damage: Research has indicated that sleep apnea may lead to measurable brain damage. Areas affected include those responsible for mood regulation, memory, and cognitive function. This damage may be due to the reduced oxygen supply during apneic events.
Increased Risk of Dementia: Studies suggest a link between obstructive sleep apnea and an increased risk of developing Alzheimer’s disease and other forms of dementia. Managing sleep apnea may help mitigate this risk.
Treatment and Management
Effectively treating sleep apnea is crucial for alleviating these psychological and neurological impacts. Continuous Positive Airway Pressure (CPAP) therapy, the most common treatment, helps maintain open airways and reduce sleep disturbances. Lifestyle changes, such as weight management and alcohol moderation, are also beneficial. In some cases, mental health treatment for associated depression or anxiety can improve overall outcomes and enhance quality of life.
Understanding the full scope of sleep apnea’s impact on psychological and neurological health emphasizes the importance of seeking treatment. Early intervention can significantly reduce risks and improve both mental health and cognitive function. The subsequent sections will discuss various treatment options in detail, highlighting ways to manage and potentially reverse the complications associated with sleep apnea.

Treatment Options for Sleep Apnea
Effective management of sleep apnea is crucial to mitigate its health risks and improve quality of life. There are several treatment options available, ranging from lifestyle modifications to medical devices and surgery. The choice of treatment depends on the severity of the condition and the specific needs of the individual.
Lifestyle Changes
Weight Management: Obesity is a major contributor to obstructive sleep apnea. Losing weight can significantly reduce the number of apneic events per night.
Exercise: Regular physical activity can improve sleep apnea by strengthening the muscles of the throat, which helps keep the airway open during sleep.
Alcohol and Smoking: Avoiding alcohol and smoking can reduce the severity of sleep apnea. Alcohol relaxes the throat muscles that control breathing, while smoking increases inflammation and fluid retention in the airway.
Positional Therapy: For some people, sleep apnea episodes are more frequent when sleeping on the back. Sleeping on the side can help keep the airway open and reduce apnea episodes.
Medical Devices
CPAP (Continuous Positive Airway Pressure): The most common treatment for moderate to severe obstructive sleep apnea, a CPAP machine uses a hose and a mask or nosepiece to deliver constant and steady air pressure to keep the airway open during sleep.
BiPAP (Bilevel Positive Airway Pressure): Similar to CPAP, but the BiPAP provides two levels of air pressure: a higher pressure when you breathe in and a lower pressure when you breathe out, which can be more comfortable for some users.
Oral Appliances: These devices, fitted by a dentist, help keep the throat open. Oral appliances may be a good choice for people with mild to moderate obstructive sleep apnea who cannot tolerate CPAP.
Surgical Options
Uvulopalatopharyngoplasty (UPPP): This surgery removes tissue from the rear of your mouth and top of your throat. Your tonsils and adenoids may be removed as well to enlarge your airway.
Maxillomandibular Advancement: In this procedure, the jaw is moved forward from the remainder of the face bones. This enlarges the space behind the tongue and soft palate, making obstruction less likely.
Inspire Therapy: A more recent treatment, Inspire therapy involves the surgical implantation of a device that stimulates the nerve controlling the tongue, keeping it in position to maintain an open airway.
Choosing the Right Treatment
The appropriate treatment for sleep apnea should be determined in consultation with a healthcare provider, who can recommend the best options based on the severity of the sleep apnea and the patient’s overall health, lifestyle, and preferences. Regular follow-ups are essential to assess the efficacy of the chosen treatment and make adjustments as needed.
Managing sleep apnea is a long-term commitment that may require combining several treatments to achieve the best results. Adhering to treatment can significantly reduce the risk of health complications associated with untreated sleep apnea, such as cardiovascular disease and diabetes, and can greatly improve quality of life. The next sections will explore strategies for managing sleep apnea effectively and the latest advances in treatment research.
Managing Sleep Apnea to Improve Life Expectancy
Effective management of sleep apnea is essential not only for improving daily functioning and quality of life but also for extending life expectancy. Here are some strategies to effectively manage this condition:
Consistent Use of CPAP
Continuous Positive Airway Pressure (CPAP) is the leading treatment for moderate to severe sleep apnea. Consistent use of CPAP machines drastically reduces the symptoms of sleep apnea, such as daytime sleepiness and cognitive impairment, and is associated with a decrease in the risk for cardiovascular diseases and other serious health issues.
- Adherence: Many patients find CPAP machines uncomfortable at first, but with regular use and adjustments, the benefits often outweigh the discomfort.
- Regular Maintenance: Keeping the CPAP device clean and replacing parts as needed can ensure the effectiveness of the therapy and prevent side effects such as nasal congestion or skin irritation.
Lifestyle Modifications
Making lifestyle changes can significantly improve symptoms and the effectiveness of other treatments:
- Weight Loss: Even a modest reduction in weight can improve or potentially eliminate obstructive sleep apnea symptoms in overweight patients.
- Exercise: Regular physical activity can improve overall health and strengthen respiratory muscles, helping to maintain open airways.
- Avoiding Alcohol and Sedatives: These substances can relax the muscles in the throat, worsening obstructive sleep apnea.
- Smoking Cessation: Smoking can increase inflammation and fluid retention in the throat, worsening sleep apnea.
Alternative Therapies
For those who struggle with CPAP therapy, alternative options may be necessary:
- Oral Appliances: These devices, designed to keep the throat open during sleep, can be effective for mild to moderate sleep apnea.
- Positional Therapy: If sleep apnea symptoms are primarily experienced when sleeping on the back, positional therapy can help. Special devices can prevent patients from sleeping in this position.
- Surgery: In certain cases, procedures to remove excess tissue or adjust anatomical abnormalities can provide long-term relief.
Regular Monitoring and Adjustments
- Sleep Studies: Regular follow-up sleep studies can help to monitor the effectiveness of the current treatment plan and make necessary adjustments.
- Consultations with Sleep Specialists: Ongoing consultations can help to address any new symptoms or compliance issues, ensuring that treatment remains effective over time.
Education and Support
- Patient Education: Understanding sleep apnea and its potential health impacts can motivate patients to stick with treatment and make necessary lifestyle adjustments.
- Support Groups: Many patients find support groups helpful for managing sleep apnea. Sharing tips and experiences can provide practical advice and emotional support.
Adopting a comprehensive management plan for sleep apnea is crucial for mitigating its impact on health and life expectancy. Proper treatment not only reduces the immediate symptoms of sleep apnea but also decreases the risk of developing associated severe health complications. As research progresses, new treatments and management strategies continue to emerge, offering hope and improved care for those affected by this challenging condition.

The Economic Cost of Untreated Sleep Apnea
Sleep apnea not only affects individual health but also imposes a significant economic burden on society. The costs associated with untreated sleep apnea extend beyond healthcare expenses and encompass productivity losses, accidents, and other indirect costs.
Healthcare Costs
- Diagnostic Testing: Sleep studies and other diagnostic tests required to diagnose sleep apnea can be costly.
- Medical Treatments: Continuous Positive Airway Pressure (CPAP) machines and other medical devices, as well as surgical interventions, contribute to healthcare expenditures.
- Management of Comorbidities: Sleep apnea is associated with several comorbid conditions, such as cardiovascular disease and diabetes, which require additional medical resources and treatments.
Productivity Losses
- Absenteeism: Sleep apnea often leads to daytime sleepiness and fatigue, resulting in increased absenteeism from work.
- Presenteeism: Even when individuals with sleep apnea are present at work, their reduced alertness and impaired cognitive function can impact productivity.
- Workplace Accidents: Sleep-deprived individuals are more prone to workplace accidents, leading to injuries, property damage, and lost productivity.
Motor Vehicle Accidents
- Increased Risk: Studies have shown that individuals with untreated sleep apnea are at a significantly higher risk of being involved in motor vehicle accidents due to impaired vigilance and reaction times.
- Fatalities: These accidents can result in severe injuries and fatalities, further contributing to societal costs.
Economic Impact on Partners and Families
- Caregiver Burden: Partners of individuals with sleep apnea may experience caregiver burden due to disrupted sleep and the need to monitor or assist with treatment.
- Healthcare Costs: Partners and family members may also incur healthcare costs related to their own sleep disturbances or health issues resulting from living with someone with untreated sleep apnea.
Overall Economic Burden
The economic burden of untreated sleep apnea is substantial, encompassing direct healthcare costs, productivity losses, and societal expenses related to accidents and injuries. However, investing in the diagnosis and treatment of sleep apnea can yield significant economic benefits by reducing healthcare utilization, improving workplace productivity, and preventing accidents and associated costs.
Advances in Sleep Apnea Research
Research into sleep apnea continues to advance our understanding of this complex disorder and improve treatment options. Here are some recent developments in sleep apnea research:
1. Precision Medicine
- Genetic Studies: Researchers are exploring genetic factors that may predispose individuals to sleep apnea. Identifying genetic markers can help personalize treatment approaches for better outcomes.
- Phenotyping: Sleep apnea is a heterogeneous disorder with various underlying mechanisms. Phenotyping studies aim to categorize patients based on specific characteristics, such as anatomical abnormalities or comorbidities, to tailor treatments more effectively.
2. Novel Therapies
- Upper Airway Stimulation: This therapy involves surgically implanting a device that delivers mild stimulation to the hypoglossal nerve, keeping the airway open during sleep. Recent studies have demonstrated its efficacy in reducing apnea events and improving quality of life.
- Pharmacological Interventions: Researchers are investigating medications targeting neurotransmitter pathways involved in airway control and respiratory drive as potential adjunctive therapies for sleep apnea.
3. Digital Health Technologies
- Telemedicine: The COVID-19 pandemic has accelerated the adoption of telemedicine for sleep apnea diagnosis and management. Remote monitoring devices and teleconsultations allow for more accessible and convenient care.
- Wearable Sensors: Advances in wearable technology enable continuous monitoring of sleep patterns and respiratory parameters, providing valuable data for diagnosis and treatment optimization.
4. Behavioral Interventions
- Cognitive Behavioral Therapy: Cognitive behavioral therapy for insomnia (CBT-I) has shown promise in improving sleep quality and reducing symptoms of sleep apnea. It targets maladaptive sleep behaviors and promotes healthy sleep habits.
- Oral Myofunctional Therapy: This therapy focuses on exercises to strengthen the muscles of the tongue and throat, improving airway function and reducing apnea events.
5. Biomarkers and Predictive Models
- Biomarkers of Severity: Researchers are exploring biomarkers in blood or saliva that correlate with the severity of sleep apnea. Identifying reliable biomarkers can aid in early detection and monitoring of the disease.
- Predictive Models: Machine learning algorithms trained on large datasets are being developed to predict individual risk of developing sleep apnea or to optimize treatment selection based on patient characteristics.
Sleep Apnea and Insurance Considerations
Navigating insurance coverage for sleep apnea diagnosis and treatment can be complex, but understanding your options and advocating for yourself can lead to better outcomes. Here are some key considerations when dealing with insurance and sleep apnea:
1. Diagnostic Testing
- Sleep Studies: Insurance coverage for sleep studies, such as polysomnography or home sleep apnea tests, varies depending on the type of insurance plan and individual policy. Some plans may require pre-authorization or documentation of medical necessity.
- Coverage Criteria: Insurance companies often have specific criteria for coverage of diagnostic testing, such as a documented history of symptoms or risk factors for sleep apnea.
2. Treatment Options
- CPAP Therapy: Continuous Positive Airway Pressure (CPAP) machines are a common treatment for sleep apnea. Most insurance plans cover CPAP devices and supplies, but coverage details may vary, including requirements for medical necessity and preferred suppliers.
- Oral Appliances: Insurance coverage for oral appliances used to treat sleep apnea may also vary. Some plans may cover these devices as durable medical equipment (DME), while others may require additional documentation of medical necessity.
3. In-Network Providers
- Preferred Providers: Insurance plans often have networks of preferred providers who have negotiated rates with the insurance company. Using in-network providers can result in lower out-of-pocket costs for diagnostic testing and treatment.
- Out-of-Network Coverage: If you choose to see an out-of-network provider, be aware that your insurance coverage may be limited, and you may incur higher out-of-pocket expenses.
4. Pre-Authorization and Documentation
- Pre-Authorization: Some insurance plans require pre-authorization for sleep apnea diagnostic testing and treatment. This involves obtaining approval from the insurance company before undergoing the procedure or receiving the treatment.
- Documentation: Keep thorough records of all communications with your insurance company, including pre-authorization requests, claim submissions, and explanations of benefits (EOBs). Documentation can help support your case if you need to appeal a claim denial.
5. Appeals Process
- Appealing Denials: If your insurance company denies coverage for sleep apnea diagnostic testing or treatment, you have the right to appeal the decision. Be prepared to provide additional documentation, such as medical records or letters of medical necessity, to support your appeal.
- Patient Advocacy: Consider seeking assistance from patient advocacy organizations or legal resources specializing in healthcare advocacy if you encounter challenges with insurance coverage.

FAQs About Sleep Apnea and Life Expectancy
Here are some frequently asked questions (FAQs) about sleep apnea and its impact on life expectancy:
1. How does sleep apnea affect life expectancy?
Untreated sleep apnea is associated with an increased risk of several serious health conditions, including cardiovascular disease, stroke, and diabetes. These conditions can significantly shorten life expectancy if left untreated. However, with proper management and treatment, the risks can be reduced, potentially extending life expectancy.
2. Can sleep apnea lead to death?
Severe untreated sleep apnea can increase the risk of life-threatening complications, including heart attacks and strokes, which can lead to death. Additionally, sleep apnea is associated with an increased risk of accidents due to daytime sleepiness, which can also be fatal.
3. Does treating sleep apnea improve life expectancy?
Yes, treating sleep apnea can improve life expectancy by reducing the risk of associated health complications. Continuous Positive Airway Pressure (CPAP) therapy, the most common treatment for sleep apnea, has been shown to decrease the risk of cardiovascular events and mortality.
4. How much does sleep apnea shorten life expectancy?
The exact impact of sleep apnea on life expectancy varies depending on factors such as the severity of the condition, the presence of other health conditions, and the effectiveness of treatment. However, studies have suggested that severe untreated sleep apnea may shorten life expectancy by several years.
5. Can lifestyle changes improve life expectancy for individuals with sleep apnea?
Yes, adopting healthy lifestyle habits can help improve life expectancy for individuals with sleep apnea. Lifestyle changes such as weight loss, regular exercise, avoiding alcohol and tobacco, and maintaining good sleep hygiene can all contribute to better overall health and longevity.
6. Are there any long-term studies on the effects of sleep apnea treatment on life expectancy?
Yes, several long-term studies have examined the effects of sleep apnea treatment on life expectancy. These studies have consistently shown that effective treatment of sleep apnea, particularly with CPAP therapy, can reduce the risk of mortality and improve overall life expectancy.
Conclusion
Sleep apnea is a prevalent sleep disorder with significant implications for both health and longevity. From its impact on cardiovascular health to its association with cognitive impairment and reduced life expectancy, untreated sleep apnea can have serious consequences. However, there is hope.
Advancements in sleep apnea research have led to improved diagnostic tools, treatment options, and management strategies. From precision medicine approaches to novel therapies and digital health technologies, there are now more options available than ever before for effectively managing sleep apnea and improving quality of life.
It’s essential for individuals with sleep apnea to seek proper diagnosis and treatment, as well as to make lifestyle changes that support overall health and well-being. By understanding the importance of adhering to treatment, advocating for appropriate care, and staying informed about the latest research findings, individuals with sleep apnea can take control of their health and potentially extend their life expectancy.
Remember, managing sleep apnea is a journey that requires dedication and perseverance, but the rewards are well worth it. By prioritizing sleep health and addressing sleep apnea, individuals can enjoy better sleep, improved overall health, and a brighter future ahead.
























Comments are closed.